Immune-Mediated Necrotizing Myopathy (IMNM)
Immune-Mediated Necrotizing Myopathy (IMNM)
What is immune-mediated necrotizing myopathy?
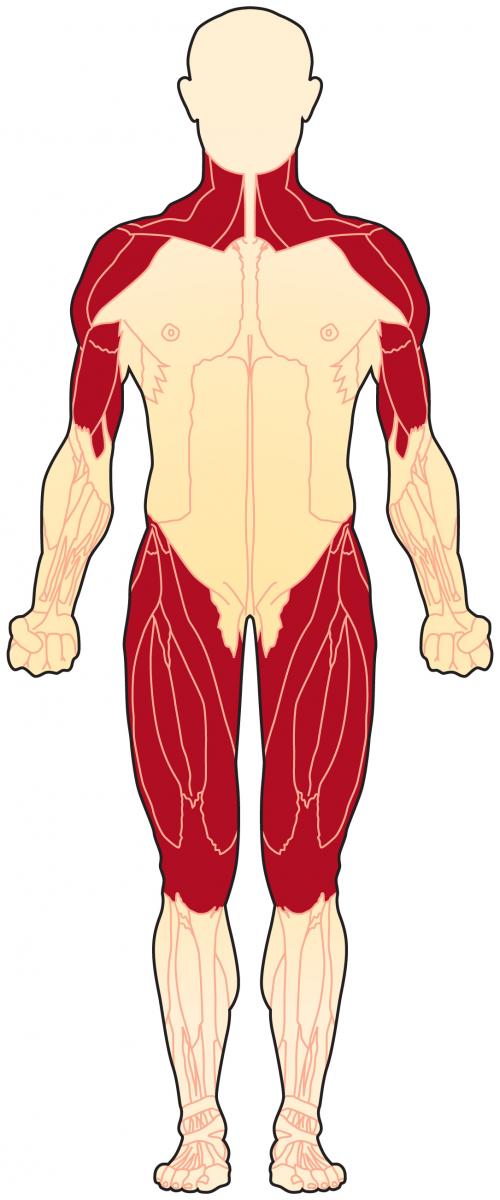 Immune-mediated necrotizing myopathy (IMNM) is one of the idiopathic inflammatory myopathies (IIMs), a group of muscle diseases that involves inflammation of the muscles or associated tissues. The IIMs are sometimes referred to as simply “myositis.” It has become clear, however, that many forms of myositis exist. IMNM is characterized by severe weakness in the proximal (close to the shoulder and pelvic girdle) muscles, usually with little effect on other parts of the body.
Immune-mediated necrotizing myopathy (IMNM) is one of the idiopathic inflammatory myopathies (IIMs), a group of muscle diseases that involves inflammation of the muscles or associated tissues. The IIMs are sometimes referred to as simply “myositis.” It has become clear, however, that many forms of myositis exist. IMNM is characterized by severe weakness in the proximal (close to the shoulder and pelvic girdle) muscles, usually with little effect on other parts of the body.
Key words
idiopathic: refers to a disease for which the cause is not known
inflammation: response of the body’s immune system to cell damage
myopathy: a muscle disease
myositis: an inflammatory muscle disease (myo means muscle, and itis means inflammation)
What are the symptoms of immune-mediated necrotizing myopathy?
The hallmark feature of people with IMNM is the presence of proximal muscle weakness. Most affected people experience only weakness, and the presence of other (extra-muscular) symptoms, such as skin or lung manifestations, suggests that they may have another type of IIM rather than IMNM.
Myositis autoantibody tests can be helpful for diagnosing an IIM and determining the prognosis of a person with the disease. Myositis specific autoantibodies (MSAs) are classically associated with distinct clinical presentations. In IMNM, two MSAs, anti-HMGCR and anti-SRP have been associated with muscle biopsies that show significant necrosis (cell death) or an immune-mediated necrotizing myopathy.
For more, see Signs and Symptoms.
What causes immune-mediated necrotizing myopathy?
In most cases, the cause of an IIM is unclear. For some reason, the body’s immune system turns against its own tissues in an autoimmune process. In IMNM, this autoimmune process leads to the necrosis (death) of muscle fibers. This necrosis can be reversible if treatment is started early.
IMNM is not a genetic disorder, although there may be genetic factors that make it more or less likely that an IIM will develop. For more, see Causes/Inheritance.
What is the progression of immune-mediated necrotizing myopathy?
Both anti-SRP and anti-HMGCR IMNM can occur in adults. Anti-SRP and anti-HMGCR IMNM present with slowly progressive proximal muscle weakness that is sometimes mistaken for limb girdle muscle dystrophy (LGMD). In general, anti-SRP and anti-HMGCR myopathy are more common in women.
In comparison to people with other IIMs, people with IMNM often experience more severe muscle weakness and present with disease that is more resistant to intense immunosuppressive treatment. Furthermore, younger people that develop anti-SRP or anti-HMGCR IMNM seem to have a worse prognosis than older people with the disease.
What is the status of research in immune-mediated necrotizing myopathy?
Research studies to increase the understanding of IMNM and clinical trials of medications to treat IIMs are underway. For a list of IMNM clinical trials, see MDA's Clinical Trials Finder Tool.
References
- Dalakas MC. Inflammatory Muscle Diseases. Longo DL, ed. N Engl J Med. 2015;372(18):1734-1747. doi:10.1056/NEJMra1402225
- Pinal-Fernandez I, Casal-Dominguez M, Mammen AL. Immune-Mediated Necrotizing Myopathy. Curr Rheumatol Rep. 2018;20(4):21. doi:10.1007/s11926-018-0732-6
- Allenbach Y, Mammen AL, Benveniste O, Stenzel W, Immune-Mediated Necrotizing Myopathies Working Group. 224th ENMC International Workshop:: Clinico-sero-pathological classification of immune-mediated necrotizing myopathies Zandvoort, The Netherlands, 14-16 October 2016. Neuromuscul. Disord. NMD 2018;28:87–99.
Last update: Feb 2023
Reviewed by Julie Paik, MD, MHS; Johns Hopkins University

