"By increasing our understanding of this debilitating disease, especially its causes, I am optimistic that we might be able to discover novel biomarkers or druggable targets. Ultimately, I am hoping that this knowledge will aid the development of personalized treatments that can halt, or reverse, the disease progression."
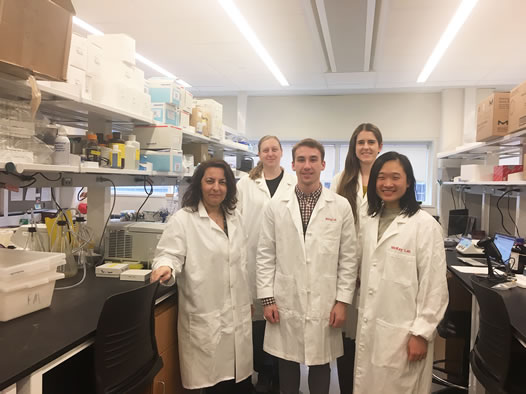
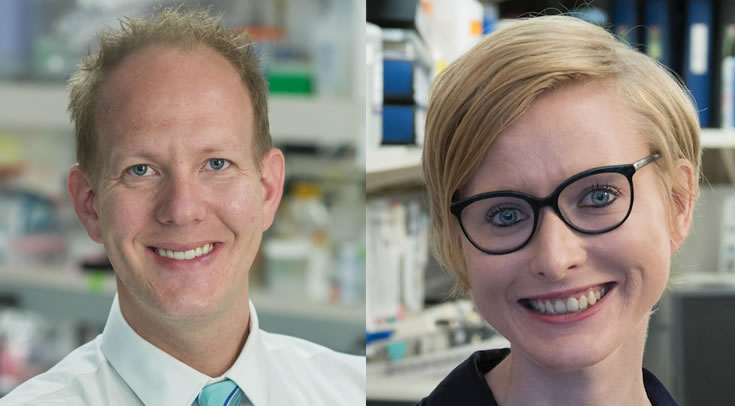
Marka Van Blitterswijk, MD, PhD, assistant professor of Neuroscience at the Mayo Clinic in Jacksonville, Fla., was awarded an MDA research grant totaling $300,000 over three years to complete an in-depth analysis of the C9ORF72 gene mutation in amyotrophic lateral sclerosis (ALS) patients and determine whether the size of the mutation can be used as a biomarker to predict factors such as survival time and cognitive changes. This work is a collaboration between the labs of Dr. Van Blitterswijk and Mark Ebbert, PhD, assistant professor of Neuroscience at the Mayo Clinic.
Although most cases of ALS are sporadic, meaning there is no family history of the disease, about 10 percent of cases are familial, meaning the disease runs in the family. Recently, it was discovered that a mutation in the C9ORF72 gene where one segment of the gene is repeated too many times — also known as a repeat expansion — is the most common cause of the familial form of ALS and is also found in some sporadic cases as well.
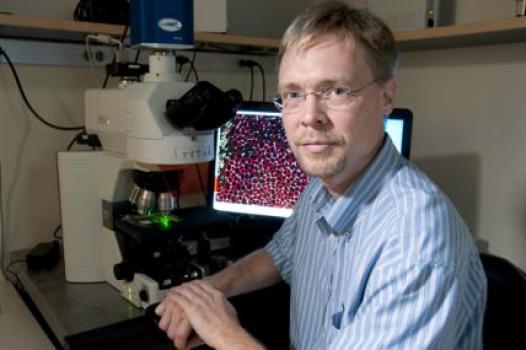
Discovery of the C9ORF72 repeat expansion has provided some knowledge of disease mechanism, but it’s still unknown how or whether interruptions in the repeated genetic material affect disease variability, development, and progression. In previous work, Dr. Van Blitterswijk acquired a large amount of clinical and pathological data from ALS repeat expansion patients, creating one of the world's largest collections of this type of information. In this study, she will use a novel technology called long-read single-molecule real-time (SMRT) sequencing on these clinical samples to determine the repeat’s exact size, whether it is interrupted, whether other changes to the DNA exist in addition to the repeated segments, and whether it is stable over time. This work could eventually pave the way for future therapies and diagnostics based on the variability found in the repeat expansion.
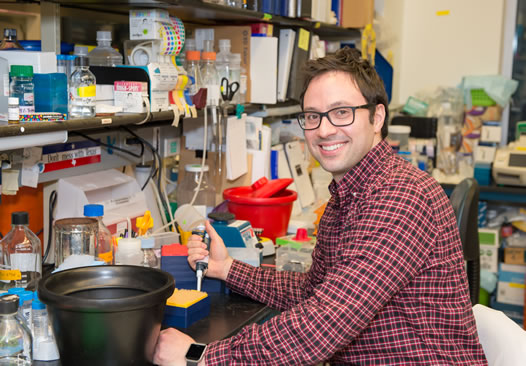
Grantee: ALS - Marka Van Blitterswijk, MD, PhD
Grant type: Research Grant
Award total:
Institution:
Country: