
All Choked Up
It’s not uncommon in ALS for something unexpectedly and abruptly to aggravate your airway and throw you into a choking fit. I know from personal experience that these choking, gagging, gasping spells are physically exhausting, frustrating and upsetting for both the choker and the caregiver.
The actions to take for choking depend on the type of choking spell you’re having. For example:
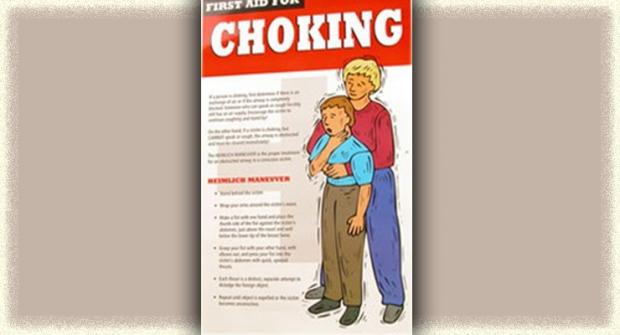
The Heimlich Choke: A large piece of food completely blocks the airway. You can’t speak or cough. This is an emergency! It requires the Heimlich maneuver, either by a caregiver or self-administered, to force the blockage up and out. If not successful in two tries, call 911 and continue trying the Heimlich while waiting for help.
Prevention is the key here. Take care to monitor the consistency of your food. Cut everything into small pieces and take smaller mouthfuls. Bread and melted cheese are especially likely to form large “plugs.” Alcohol, talking or other distractions while eating increase the risk of choking.
The Damn-Near Heimlich Choke: A pill or bit of food sticks in your throat. After a moment you can breathe but with a scary “heeee” sound.
Just as you start getting a little air in, you start coughing and/or gagging again. Over and over.
You can feel the darn thing stuck in your throat teetering between sliding up and making you gag and sliding down and making you cough. Scary, exhausting, but you can get a breath in between coughing spells.
The Heimlich or assisted cough technique may help. Focus on getting the obstruction up and out, not down the throat, because of the danger that it will lodge more firmly or go into the lungs. Therefore, avoid back whacking!
Talk with your clinic team about techniques appropriate for you and your caregiver’s strength. People with even minimal swallowing problems should never eat when home alone.
If you choke almost every time you eat and mealtimes are a dreaded experience, it’s time to get evaluated for a feeding tube. Besides the physical stress of a choking attack, the real danger of suffocation and the loss of calories due to fear of eating, choking can lead to aspiration, in which food or pills go into the lungs and cause life-threatening pneumonia.
The Foodless Sneaky Choke: You’re just sitting there minding your own business or even snoozing when suddenly you’re coughing and choking. A simple swallow of saliva goes awry and sends your larynx (vocal cords) into a spasm that closes off your airway. This is called a laryngospasm and isn’t uncommon in ALS. You fight to inhale but nothing happens. You can’t take a breath, can’t call for help, and panic crashes over you.
After an eternity, you finally suck in a thin, wheezing, tiny “eeee” breath. Slowly the spasm eases. The only thing I’ve found that helps me through these is the hard-learned lesson that they’re intense but short-lived. You’re not really choking, you can get some air, and the spasm will ease in just a moment or two.
Common causes of laryngospasm in ALS are liquid or saliva that went the wrong way into the larnyx, acid reflux disease, smoke, strong smells, emotion, alcohol, cold or rapid bursts of air, and even spicy foods.
Some techniques that may help ease the spasm include:
- Breathe through your nose rather than mouth.
- Pull in a breath from lower down, inflating your belly rather than breathing shallowly.
- When exhaling, very lightly blow out a sustained breath, like a soft whistle without puckering the lips.
- Swallow repetitively.
Caregivers can help by giving calm reassurance, gentle back rubbing (not whacking)and other support in riding out the spasm.
The Phlegm from Hell Choke: You try to clear your throat. Hrrrmph. Hrrrrrrrrmph. No good. Over and over you try to break up and cough out the thick clog in the back of your throat until you’re worn out and gasping.
My treatment is to take a dose of papaya juice or expectorant (guaifenesin, available over the counter) to thin the secretions. Then I lie down (BiPAP on) and have my caregiver do an assisted cough or use a cough assist machine. By lying down, I don’t have to fight gravity to bring the mucus up. Staying well hydrated can help keep secretions thinner.
The Nonchoke Sticker: A pill or bit of tortilla chip sticks on the way down and sits there feeling like a thorn in your throat. This little sucker can hurt for a day or more. After taking a small sip to make sure I can still swallow, I try taking the longest drink I can. Sometimes this repeated swallowing does the trick.
Advice to Caregivers
In any choking situation, fake being calm and quickly go through a list of possible actions. Ask, “Do you need a Heimlich? Assisted cough? A drink? Cough medicine? Suction?”
As with any aspect of ALS, always discuss choking concerns with your doctor. It’s good to practice the Heimlich and assisted cough techniques before you need to use them. For more information on these techniques, contact your local MDA/ALS center or MDA clinic.
Editor’s Note: Diane Huberty, of Fort Wayne, Ind., is a former neurology head nurse/instructor who has had ALS for more than 20 years. She writes about tips for living with ALS. MDA Medical Director Valerie Cwik and Senior Writer Christina Medvescek contributed to this article.