Lambert-Eaton Myasthenic Syndrome (LEMS)
Lambert-Eaton Myasthenic Syndrome (LEMS)
 What is Lambert-Eaton myasthenic syndrome (LEMS)?
What is Lambert-Eaton myasthenic syndrome (LEMS)?
Lambert-Eaton myasthenic syndrome (LEMS) is an autoimmune disease — a disease in which the immune system attacks the body's own tissues. The attack occurs at the connection between nerve and muscle (the neuromuscular junction) and interferes with the ability of nerve cells to send signals to muscle cells.
Specifically, the immune system attacks the calcium channels on nerve endings that are required to trigger the release of chemicals (acetylcholine). With fewer calcium channels, the nerve ending releases less acetylcholine. Acetylcholine is a chemical messenger that triggers muscle contraction. In people with LEMS, the lowered levels of acetylcholine are not sufficient to cause normal muscle contractions, causing muscle weakness.
The disease is named after Edward Lambert and Lee Eaton, neurologists at the Mayo Clinic in Rochester, Minn., who first described myasthenic syndrome in the 1950s and '60s.
What are the symptoms of LEMS?
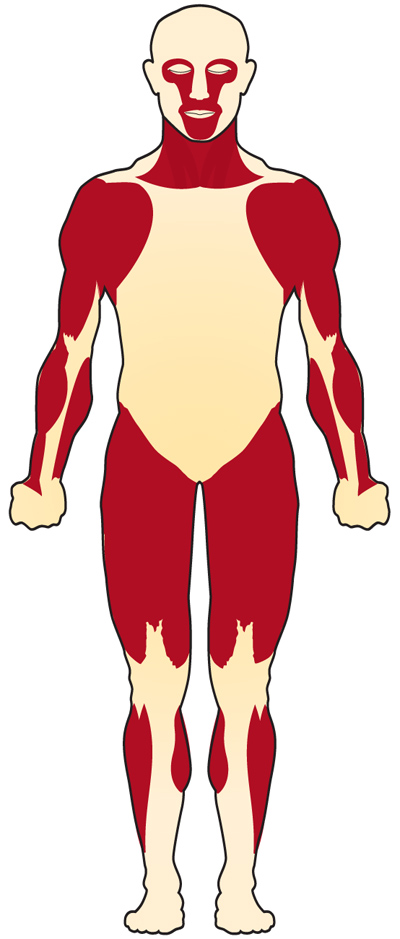
Initially, LEMS can cause weakness in the upper legs and hips, leading to difficulty walking, and weakness in the upper arms and shoulders, which can make self-care difficult. Like myasthenia gravis (MG), it also can result in weakness of the eye muscles and those involved in talking, swallowing, and chewing, but these symptoms are usually mild.
In addition, most people with LEMS also have some autonomic (involuntary) nervous system dysfunction (dry mouth is the most common symptom), although this aspect of the disease is not usually a defining feature. For more, see Signs and Symptoms.
What causes LEMS?
In about 50-60% of cases, LEMS is associated with an underlying cancer, particularly small cell lung cancer. It is thought that the body's attempt to fight cancer inadvertently causes it to attack nerve endings because cancer cells share some of the same proteins as nerve endings.
In the other 40-50% of cases, the cause is unknown and is thought to result from a primary autoimmune process. For more, see Causes/Inheritance.
What is the progression of LEMS?
There are two forms of LEMS, each with a different average age of onset and cause but with the same underlying change in the body that leads to the disease.
One form is associated with small cell lung cancer (most often caused by long-term cigarette smoking). It has an older age of onset (average 60 years) and is caused by an accidental attack on the nerve terminal by the immune system as it attempts to fight the cancer. In this form of LEMS, successful treatment of the cancer removes the trigger for LEMS and may result in recovery from LEMS.
The second form is not associated with cancer. It may have a genetic component linked to autoimmunity and it has two peak ages of onset, one around 35 years and another later in adulthood around 50–54 years.
In both forms of LEMS, the disease is caused by the immune system making antibodies against calcium channels on the nerve endings, leading to muscle weakness. LEMS symptoms can usually be managed with symptomatic therapies that help relieve weakness and immune-modulating treatments that reduce the immune system’s attack on the nerves.
What treatments are available for LEMS?
The most common treatment for LEMS is 3,4-diaminopyridine (3,4-DAP) (brand name Firdapse), a medication that helps nerves release more of the neurotransmitter acetylcholine to improve signaling to muscles and thus improve muscle strength. If symptoms are still not well controlled or are severe, additional treatments may be used, such as intravenous immunoglobulin (IVIG), plasmapheresis, or immune-suppressing medications. If LEMS is associated with cancer, treating the cancer can also help improve the symptoms of LEMS.
What is the status of research on LEMS?
Scientists are uncovering why the immune system in LEMS mistakenly attacks the nerves and how this damage occurs, while also developing new treatments that may strengthen signals at the nerve and muscle junction (neuromuscular junction) or lessen the need for long-term immune-suppressing medicines. At the same time, researchers are also working on improving diagnostic tests to identify LEMS earlier and more accurately, including better tools to detect cancers that can sometimes be associated with this condition.
Additional reading
- Kesner VG, Oh SJ, Dimachkie MM, Barohn RJ. Lambert-Eaton Myasthenic Syndrome. Neurol Clin. 2018 May;36(2):379-394. doi: 10.1016/j.ncl.2018.01.008. PMID: 29655456; PMCID: PMC6690495.
- Varon MC, Dimachkie MM. Diagnosis and treatment of Lambert-Eaton myasthenic syndrome. Practical Neurology (US). 2024;23(3):26-28,47.
Last revised December 2025.

