Advances in Inclusion-Body Myositis
The least understood inflammatory myopathy is finally yielding to researchers' probes
On winter mornings in icy Prescott, Wis., Ed Bankston gets up early, and, as he has done for many years, drives to his office in St. Paul, Minn. Bankston, 55, has been an attorney with the St. Paul District of the U.S. Army Corps of Engineers since 1988, and he now heads the district's legal department.
But getting to his desk requires a little more planning than it once did. Nowadays, Bankston drives an adapted Dodge Caravan with hand as well as foot controls to an underground garage, where a staff member meets him with a power wheelchair. In the evening, he drives the chair back down to the garage and transfers into his van.
Walking is something Bankston has all but given up, except to get into the shower, which requires two forearm crutches. His arms and hands are weak,making it hard to hold onto objects or to open containers.
The trouble started in his late 40s, when Bankston began feeling that his muscles were no longer as strong as they once were. "If I was trying to play tennis or bicycling and tried to stop, my knee would buckle, and I would fall," he recalls. "And I couldn't walk as fast as I used to. At first, I thought I was just getting older."
But in 1994, at age 49, he grew concerned enough to consult his internist. The doctor told him his strength was within normal limits for his age, but the weakness continued — and progressed.
A year or so later, Bankston and his wife, Pam, went to a neurologist, who did an electromyogram and made a diagnosis of amyotrophic lateral sclerosis (ALS, or Lou Gehrig's disease), a devastating disease of muscle-controlling nerve cells that usually leads to death within a few years.
 The Bankstons decided to get a second opinion and made an appointment with the Mayo Clinic in Rochester, Minn. Fortunately, they received a lesser sentence: Bankston was told he either had polymyositis (PM), a disorder involving an immune system attack on muscle; or inclusion-body myositis — IBM — a muscle disorder that major medical centers were just beginning to recognize.
The Bankstons decided to get a second opinion and made an appointment with the Mayo Clinic in Rochester, Minn. Fortunately, they received a lesser sentence: Bankston was told he either had polymyositis (PM), a disorder involving an immune system attack on muscle; or inclusion-body myositis — IBM — a muscle disorder that major medical centers were just beginning to recognize.
How rare is it?
Until recently, IBM was considered a rare disease, but experts now say it's the most common form of inflammatory muscle disease in men over age 50. Some even say it may be the most common muscle disease of any kind that begins in either men or women over 50.
IBM is more common in men but affects both sexes. The slowly progressive disease produces severe weakness and muscle atrophy (shrinkage) in the forearms, including the muscles controlling finger movements. It typically affects the muscles of the arms and legs, particularly the thigh (quadriceps) muscle and muscles in the lower legs that move the feet. The weakness isn't necessarily the same on both sides of the body. About one-third of those affected have weak throat muscles and difficulty swallowing.
The usual type of IBM isn't considered a genetic disorder (although genetic risk factors may be involved) and is called sporadic IBM. There are also genetic forms, which present a slightly different picture (see When It Runs in the Family section below).
"They started treating me with Imuran and prednisone because they thought that would differentiate which disease it was," Bankston says. Both medications suppress the immune system. "If it was polymyositis, they thought it would respond. After three or four months, we discontinued the treatments, because it didn't respond, so they pretty much figured it was inclusion-body myositis."
About a year later, the Bankstons traveled to the National Institutes of Health in Bethesda, Md., where the diagnosis of IBM was confirmed. (Last year, MDA began covering the disease in its services program.)
Curious inclusions
None of Bankston's story is a great surprise to Valerie Askanas, an MDA-supported researcher and clinic director at the University of Southern California in Los Angeles.
Askanas is among a handful of scientists now mapping the territory of sporadic and hereditary forms of IBM and separating it from other types of inflammatory myopathies (muscle disorders involving an immune-system reaction known as inflammation), muscular dystrophies and diseases of the nervous system, like ALS.
The name itself is a mouthful, as Askanas is the first to admit. An inclusion, or inclusion body, she says, is "a cluster of material, anything that doesn't belong inside a cell. It has a broad meaning. In IBM, we're constantly discovering new proteins in the inclusions."
The "myositis" part of the name carries the prefix myo, which means muscle, and the suffix itis, which means inflammation.
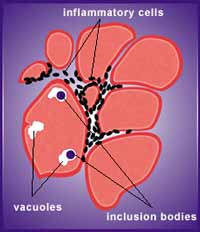
When muscle biopsy samples from people with IBM are examined under a microscope, trained eyes can see strange-looking inclusions; bubblelike spaces called vacuoles that are sometimes empty and sometimes contain inclusions; and inflammatory cells invading like enemy troops around the borders of muscle fibers. It's largely what's inside the inclusions that intrigues Askanas. Until recently, nobody was sure what they were.
"Without special staining," she says, "it was not possible to see what we see now. It was only possible to see that within the vacuoles there was some material. A few years ago, it was becoming apparent that those inclusions contained clusters of filaments. That was all that was known for many years."
Researchers also observed that the disease wasn't very treatable. "It differs from polymyositis, and that always puzzled us," Askanas says, "why polymyositis is so well treatable in many patients and why inclusion-body myositis is not."
An Alzheimer's connection?
Then, in 1990, Askanas attended a meeting in Birmingham, England, to probe the mysteries of ALS, another baffling disease. In that disorder, muscle-controlling nerve cells (motor neurons) degenerate for reasons that remain obscure. "Someone was showing inclusions in neurons, and they were staining positively for ubiquitin," Askanas recalls.
 Shortly before leaving for Birmingham, Askanas had been studying a muscle biopsy sample from a patient with suspected IBM. "I remembered how they looked," she says of the IBM inclusion bodies she'd seen there. At the meeting, she says, "they were still very much in my eyes."
Shortly before leaving for Birmingham, Askanas had been studying a muscle biopsy sample from a patient with suspected IBM. "I remembered how they looked," she says of the IBM inclusion bodies she'd seen there. At the meeting, she says, "they were still very much in my eyes."
Askanas began wondering if the muscle inclusions might also be positive for ubiquitin, a protein that tags other proteins for cellular degradation. Ubiquitin had also shown up in brain tissue in another degenerative disorder, Alzheimer's disease. "When I came back from the meeting, I did the staining — and the IBM inclusions were incredibly positive."
About the same time, neuromuscular disease specialist and MDA research grantee Jerry Mendell at Ohio State University in Columbus was also becoming intrigued with IBM pathology. In 1991, Mendell and colleagues published a paper showing that amyloid, a compound composed of malformed protein pieces that take up a special stain, could also be found inside the muscle fibers of people with inclusion-body myositis.
Amyloid had by then been associated with brain degeneration in Alzheimer's and had been seen in some other conditions, but it had never before been shown to exist inside muscle fibers. "When Jerry showed this in 1991, many people didn't believe it," Askanas says. "But we looked, and indeed it was there."
Later, she and neurologist W. King Engel, her husband and colleague, identified amyloid beta, a protein fragment cleaved off from a larger protein known as amyloid beta precursor protein, as a major component of the amyloid deposits in IBM. This same protein has been implicated in the abnormal deposits in Alzheimer's brain tissue (where it's outside, not inside, brain cells).
Askanas' team went on to identify several more proteins found in the mysterious inclusion bodies in the muscle fibers of people with IBM. Curiously, many of these proteins — for example, amyloid beta, apolipoprotein E, ubiquitin, and possibly a toxic form of a protein known as tau (one with too many phosphate groups) — are also found in the brains of people with Alzheimer's, leading the investigators to suspect there might be some biochemical pathway common to the two disorders.
But here Askanas wants to clear up what she fears has become a frightening rumor: "We personally have never seen IBM patients with Alzheimer's disease; nor have our colleagues I have talked to. That's very important. I'm not so brave as to say that IBM protects against Alzheimer's disease, but I can say that IBM does not predispose one to Alzheimer's.
"In regard to IBM, I'm developing a hypothesis now that there are predisposing genes to different diseases, not disease-causing genes but disease-predisposing genes, and that there's one set that predisposes people to IBM and a different set that predisposes them to Alzheimer's disease. What I think is happening is that some genes direct a disease process to occur in aging muscles, and another set of genes directs a disease process to occur in the aging brain."
|
||||||
In fact, the mysteries of IBM aren't limited to its similarities to Alzheimer's brain tissue, Askanas notes. Another clue to the disease may lie in what she and Engel have called junctionalization. Normally, Askanas notes, the proteins produced at the neuromuscular junction — the place on each muscle cell that receives contact from a nerve cell — are unique to that cellular domain and aren't made elsewhere in the mature muscle fiber (cell). In IBM muscle samples, such "junctional" proteins appear all over the cell, not just at the junctions. That, Askanas believes, represents some sort of cellular process run amok.
Searching upstream
While amyloid beta, tau and various mislocated proteins are clearly key parts of the picture in IBM, they probably appear "midstream" in the development of the disease, says Engel, who has worked closely with Askanas for a decade on IBM research and also sees many patients with the disease. "There's something upstream that leads to the accumulations of these proteins — and that's what is now being sought by the Askanas team."
That upstream something, Engel says, could well be a virus. "We've proposed that a virus is the real trigger. Viruses have a way of putting themselves into the cell, such that their RNA or DNA [genetic material] can be there but not in the shape of viral particles," which makes them hard to find, Engel says. A virus hasn't been detected in IBM, he notes, perhaps because the techniques being used to find it aren't sufficiently sensitive, or perhaps because it isn't there at all.
Askanas and her colleagues are also looking at another phenomenon that could play a role in IBM — the aging process itself. "There may be something about the aging muscle fiber environment that's not ordinarily a problem, but that could allow a virus contracted decades before to become detrimental," Engel says.
'Itis' not forgotten
 While Askanas and Engel have focused on aging and inclusions, other investigators have looked closely at the myositis part of IBM.
While Askanas and Engel have focused on aging and inclusions, other investigators have looked closely at the myositis part of IBM.
Neurologist and MDA research grantee Rabi Tawil, who co-directs the MDA clinic at the University of Rochester Medical Center in upstate New York, believes treating the inflammatory component of IBM still holds promise.
Tawil admits that attempts to treat IBM with various anti-inflammatory and immunosuppressant drugs have been far from successful. Corticosteroids (the prednisone family of drugs) allow some people to "transiently improve," he says, "but they don't sustain the improvement." Other treatments aimed at the immune system, including intravenous immunoglobulins — a cumbersome and somewhat risky way of changing the behavior of the immune system — have likewise failed, Tawil notes.
But he and several researchers are far from giving up on the idea that the immune system is a key player in sporadic IBM.
"Some investigators believe IBM is a degenerative myopathy [muscle disorder] and that the inflammation that's present is a kind of nonspecific inflammation but not the primary insult. But there's also some pretty significant evidence that IBM is an immune-mediated [immunologically caused] myopathy," he says.
While Askanas and Engel have focused on the parallels between IBM and Alzheimer's, Tawil and colleagues have chosen to look at the similarities that may exist between IBM and multiple sclerosis, a disorder in which it's believed that the immune system mistakenly attacks the myelin coating that forms a sheath around nerves. "In parallel to MS," Tawil notes, "IBM does not seem to respond to the typical immunosuppressive agents."
One new type of agent to which MS has responded, however, is a class of drugs called interferons, which are naturally produced cellular proteins that have regulatory effects on the immune system. Tawil has chosen to investigate interferon beta-1a, marketed as a treatment for MS by Biogen under the trade name Avonex. The drug is given by intramuscular injection once a week.
 With help from MDA, the National Institutes of Health and Biogen, Tawil and colleagues have recently completed a small trial of Avonex in IBM. "There was concern about whether giving something intramuscularly to somebody with atrophic muscle might be a limitation," he says. "But we've been able to work around that by having patients give injections in a different limb every week and choose only the best-suited muscles."
With help from MDA, the National Institutes of Health and Biogen, Tawil and colleagues have recently completed a small trial of Avonex in IBM. "There was concern about whether giving something intramuscularly to somebody with atrophic muscle might be a limitation," he says. "But we've been able to work around that by having patients give injections in a different limb every week and choose only the best-suited muscles."
Although no one showed dramatic improvement, the drug was safe and well tolerated. The research team now plans to move on to a seven-center study and to give the drug at double the dose. "There's some evidence that higher doses of interferon beta may have additional beneficial effects," Tawil says, noting that recruitment for the trial will begin when all the regulatory matters have been settled.
Confusion and frustration
Neuromuscular disease specialist Richard Barohn at the University of Kansas calls IBM a frustrating disease for patients. Barohn, who has been an MDA research grantee and an MDA clinic director at the University of Texas in Dallas and San Antonio, will coordinate the Kansas City part of the interferon trial.
 "Most folks have gone many years before getting diagnosed," he says. "The average length of time in our study was eight years. Most doctors don't know how to recognize IBM."
"Most folks have gone many years before getting diagnosed," he says. "The average length of time in our study was eight years. Most doctors don't know how to recognize IBM."
He tells people that "it's not ALS and they're not going to die from the disease. We tell them they're going to experience some disability problems, some weakness in their quadriceps muscles and in their finger and hand muscles. We have them see specialists in physical therapy, occupational therapy, all the rehabilitation specialists, and we try to help them adapt to their disabilities. Once people have some knowledge of the disease from doctors and from MDA, it goes a long way in letting them deal with it."
IBM looks like ALS in that it affects middle-aged and older people and often affects the swallowing muscles early. It looks like polymyositis in that both are inflammatory muscle diseases that involve weakness of the arms and legs. But, says Rabi Tawil, an experienced clinician doesn't have too much trouble telling the difference — even before seeing a biopsy sample.
While PM affects females more often than males and doesn't particularly target older adults, IBM affects males more often than females and usually strikes after 50. In PM, the weakness is mostly in the proximal muscles, those closest to the center of the body, such as the hip and shoulder muscles, while in IBM, weakness of the distal (far from the center) muscles is at least as great.
"When you've seen IBM patients, you can pick them out even before you see the biopsy," Tawil says. "They have distal weakness, finger flexion weakness, and selective weakness of the quadriceps muscle. They sometimes also have swallowing problems. Often, people with suspected polymyositis are treated with corticosteroids, and often they don't get better. Two or three years later, they have another biopsy and their 'steroid-resistant polymyositis' turns out to be inclusion-body myositis."
Therapies and devices
Treatment for IBM is, unfortunately, not very effective, and the verdict on exercise isn't in yet. Barohn encourages people to walk or swim while they can, but he doesn't try to force an exercise program.
"Usually, when people with IBM lose the ability to walk with a cane or walker, they go to a motorized scooter," Barohn says, noting that a wheelchair isn't always needed. He sometimes recommends bracing some of the finger muscles, but he hasn't found leg braces to be very useful in IBM. Swallowing problems can be overcome with the help of a speech therapist.
Engel takes a similar approach, perhaps being a little more likely to try prednisone. "We've had some patients who are distinctly improved on it, in a sustained way, and a number of patients who are not," he says. Engel has also found that intravenous immunoglobulins help some people with IBM if they're given in adequate amounts and often enough.
Engel encourages IBM patients to use a walker when leg weakness and lack of grip strength make canes unsafe for support. He's seen too many falls with broken bones, including a fatal skull fracture in one person with IBM, he says.
When it comes to exercise, Engel advises people to take an "intuitive approach," noting that the subject really hasn't been studied. "If you're exhausted by the exercise, don't do that much the next time," Engel says. "Mild exercise is appropriate. If the muscle feels sore afterwards, then it's too much." Swallowing muscles can sometimes be aided by prednisone, he says, as well as by dilation of the esophagus by a specialist.
Aging population, aging muscles
 "In the 21st century, people are going to live to be older, to 85 or 90 as a normal phenomenon," Askanas says. "We have an aging cell in this disease, but we know very little about aging muscle in general. We need to learn more. We're going to see a lot of diseases associated with aging. IBM is one, but there are more."
"In the 21st century, people are going to live to be older, to 85 or 90 as a normal phenomenon," Askanas says. "We have an aging cell in this disease, but we know very little about aging muscle in general. We need to learn more. We're going to see a lot of diseases associated with aging. IBM is one, but there are more."
Research in IBM will benefit research in other disorders of aging, Askanas believes, just as research in those disorders may help IBM researchers make progress. For the present, Askanas and many others are trying to leave no stone unturned. She and several colleagues recently published a paper that suggests yet another lead: The mitochondria — cellular powerhouses that produce energy — in IBM muscle samples frequently contain an abnormality that may be of some importance, although it isn't yet clear where this finding fits into the whole picture.
Finding the genes that cause hereditary IBM will open new doors to all forms of the disease, Askanas notes, just as finding a genetic mutation that can cause ALS has had implications for the nongenetic forms of that disorder. Askanas is confident that the chromosome 9 form of the disease will be demystified soon. The gene, she says, is being searched for and will "pop out" any day now.
When It Runs in the Family
Inclusion-body myositis is considered a nongenetic disease, although there may be genetic factors that predispose a person to it. This common form of IBM is known as sporadic IBM, or sIBM.
For many years, however, doctors have observed apparently hereditary muscle disorders that bear a resemblance to sIBM in certain ethnic groups, particularly Jews living in the Middle East or descended from that group. Most have been thought to originate from ancient Persia, an area today covered mostly by Iran but also encompassing Iraq, Afghanistan, Egypt and Syria. Similar muscle disorders have also been found in people of Japanese, Mexican and French Canadian heritage.
These slowly progressive muscle diseases have been called by various names over the years, including simply "progressive muscular dystrophy." They're now generally called forms of hereditary inclusion-body myopathy, or hIBM, by experts in the field. MDA classifies the hereditary forms as "distal muscular dystrophies" (because they often feature marked muscle weakness in areas away from the center of the body) and the sporadic form as an "inflammatory myopathy" (because the biopsy samples usually show inflammation).
The Persian (Iranian) Jewish form of hIBM has been linked to a small area on chromosome 9 and is thought to be inherited in a recessive pattern, meaning it takes two flawed genes (one from each parent) to produce symptoms. Hereditary IBM in Japanese and Mexican families has been linked to the same genetic area, while the disorder in French Canadians appears to result from a mutation in a different gene. In none of these groups has a specific defective gene yet been identified.
Dominantly inherited (requiring only one flawed gene) forms of hIBM also exist. A gene on chromosome 17 that codes for a muscle protein known as myosin heavy chain has been found responsible for the disorder in a Swedish family, but this disease has some unusual additional features, such as joint contractures and paralyzed eye muscles.
Hereditary IBM — mostly the chromosome 9 form, which is the most studied — usually spares the quadriceps, while sIBM particularly targets this thigh muscle. Strikingly, hIBM shows itself early, often in the teens or 20s, with no gender preference, while sIBM is a disease of older people, particularly men.
Because there are so many similarities between the hereditary and sporadic forms of IBM, greater understanding of the genetic defects underlying hIBM is expected to help researchers understand all forms of the disease.
MDA Resource Center: We’re Here For You
Our trained specialists are here to provide one-on-one support for every part of your journey. Send a message below or call us at 1-833-ASK-MDA1 (1-833-275-6321). If you live outside the U.S., we may be able to connect you to muscular dystrophy groups in your area, but MDA programs are only available in the U.S.
Request Information